Optimal nutrition and digestive health are essential for overall well-being and longevity. In clinic, I often see patients suffering with IBS and bloating symptoms, and I use structural and visceral osteopathy to improve their symptoms. Working in tandem with a nutritionist can be so helpful in these cases. I’ve invited Nicolle Appleton, Nutritional Therapist at Appleton Nutrition, who works with me at 18 Charles Street, to give you some more information in this guest blog. She’ll explore how to enhance digestive wellness by understanding and supporting stomach acid production, and guide you through practical strategies to improve your digestive health.
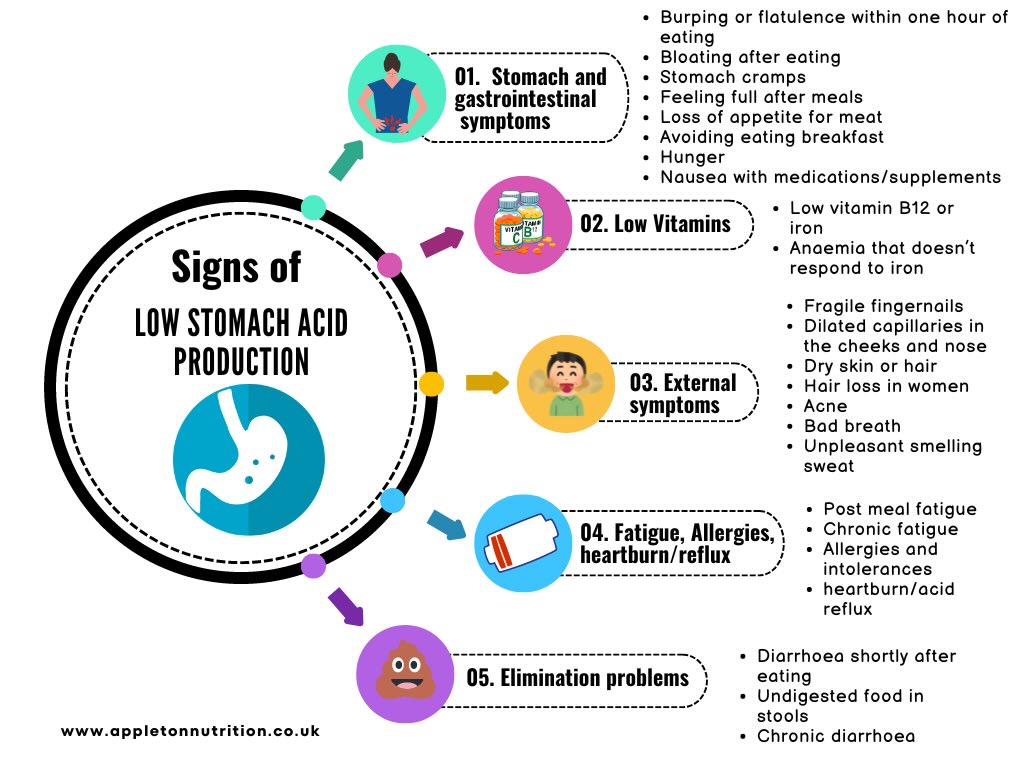
Recognising Low Stomach Acid: Common Symptoms and Indicators.
In this blog, “stomach acid” specifically refers to low hydrochloric acid (HCl), a key component of gastric juices. While “stomach acid” is often used to describe the entire contents of gastric juices, here it will focus on stomach acid levels. Stomach acid plays a crucial role in maintaining our overall health and well-being. It serves two primary functions: firstly, it acts as a barrier against harmful pathogens, preventing bugs from entering our digestive system and causing illness. Secondly, stomach acid along with gastric juices, facilitates the digestion of proteins, fats, and carbohydrates, and initiates the production of further enzymes essential for the digestive process.
While many people believe that high stomach acid is the main cause of digestive issues, it is increasingly recognised that low stomach acid, or hypochlorhydria, is a prevalent issue, especially among older adults. Low stomach acid refers to a condition where the stomach does not produce enough (HCl), resulting in a higher stomach pH and a less acidic environment. This can lead to impaired digestion, nutrient deficiencies, increased risk of infections, and gastrointestinal damage We will delve into the signs and symptoms that can help you recognize this condition, uncover the potential causes behind insufficient stomach acid production, and provide actionable tips to enhance your stomach acid levels naturally. Additionally, we will discuss various testing options, such as blood tests, stool tests, and other diagnostic methods, to help you and take informed steps towards better digestive health.
How Nutritional Therapy Can Help Address Low Stomach Acid
Direct testing for low stomach acid isn’t widely available or commonly practiced in conventional medicine. In functional medicine, particularly in nutritional therapy, we take a comprehensive approach by examining potential antecedents, triggers, and mediators of low stomach acid. Instead of relying solely on direct tests, we assess symptoms and look for related issues such as gastrointestinal infections, Small Intestinal Bacterial Overgrowth (SIBO), and vitamin and mineral deficiencies which are things we can test for. By identifying these underlying factors, we can develop targeted strategies to support and enhance stomach acid production, thereby improving overall digestive and overall health. This holistic approach ensures that we address the root causes and provide personalised care based on a thorough understanding of your unique health profile.
Understanding Why Stomach Acid Production Declines
As we get older, our stomach lining can wear down due to long-term inflammation. This is often worsened by infections like Helicobacter pylori. This wear and tear leads to a condition called atrophic gastritis, which reduces the amount of acid the stomach can produce. Older adults often have lower levels of pepsin, a key digestive enzyme that needs stomach acid to work properly. Over time, the body becomes less able to produce and release these enzymes.
Dehydration due to insufficient blood flow to the stomach can impair stomach acid production. This affects the parietal cells responsible for producing stomach acid. Dehydration also causes elevated cortisol levels (our stress hormone), which can interfere with stomach acid production. Additionally, the mucus lining of the stomach can become too thick, further impairing stomach acid secretion. A zinc deficiency can impair stomach acid production, as zinc is essential for this process. Similarly, a lack of other necessary nutrients can also affect stomach acid levels.
Private blood testing and stool analysis
The WELLNESS ADVANCED BLOOD DRAW – £89 – includes testing for zinc, iron, B12, magnesium, and many other essential nutrients.
A stomach infection with a parasite called Helicobacter pylori can damage the stomach lining. Helicobacter pylori produces an enzyme called uric acid, which makes the stomach less acidic. For H. pylori, your GP can order a stool analysis. Alternatively, you can order the test as part of a Comprehensive Stool Analysis (GI360) for £370, or on its own for £139.
Autoimmune diseases may also be a factor, causing destruction of the parietal cells that produce stomach acid. This condition, known as autoimmune gastritis, can lead to a B12 deficiency called pernicious anaemia.
Advanced Vitamin B12 Blood Test – £89.00. A comprehensive investigation into vitamin B12 deficiency, this test includes a full blood count, as well as measurements for active vitamin B12, folate, and ferritin.
Stress leads to elevated cortisol levels that can interfere with Stomach acid production. Managing stress through relaxation techniques, exercise, and adequate sleep can help maintain healthy stomach acid levels.
Consider the Advanced Adrenal Profile for £120 to assess stress hormones. Some underlying conditions may affect stomach acid production, such as hypothyroidism or uncontrolled diabetes. Testing options like the Advanced Diabetes Blood Test (£67) for glucose levels and the Thyroid Monitor and Vitamin Home Test (£120) for thyroid function and nutrient status can provide insights for better management.
Advanced Diabetes Blood Test: Measure current glucose levels and check blood sugar control over the last 10-12 weeks (£67).
Thyroid Monitor and Vitamin Home Test: Includes a thyroid check, as well as tests for B12, iron, vitamin D, and inflammation (£120).
Diet’s importance for stomach acid production
Diet also plays a crucial role in stomach acid production. Protein is needed to release gastrin, a hormone that promotes stomach acid production. Therefore, a diet low in protein can hamper this process. Including high-quality protein sources such as lean meats, fish, eggs, and legumes can support adequate stomach acid levels. Artificial additives and preservatives can negatively affect gut flora. A healthy gut is crucial for proper digestion and stomach acid regulation, and any disruption can lead to dysbiosis, affecting stomach acid levels. These additives and preservatives can also be chemical irritants to the stomach, reducing its ability to produce stomach acid.
A high sugar diet may promote the growth of harmful bacteria and yeast in the stomach and intestines. This overgrowth can interfere with normal digestion and reduce stomach acid levels.
SIBO breath test for symptoms consistent with small intestinal bacterial overgrowth. SIBO Glucose – £168.
Refined carbohydrates are quickly digested, leading to rapid spikes and drops in blood sugar levels. These fluctuations cause stress in the body, which can interfere with acid production.
A low-fibre diet can lead to reduced gastrin levels and lower stomach acid, as fibre is essential for promoting stomach acid secretion. Low-grade inflammation, including in the stomach, can impair the function of the parietal cells responsible for stomach acid production.
Inflammation can also affect the gut-brain axis, leading to stress and anxiety known to affect stomach acid levels. Hydrogenated fats can impair the function of digestive enzymes and bioavailability; they can also cause inflammation, further disrupting the digestive process.
Top Tips to improve your digestive health
Mindful eating is crucial. Avoid distractions like TV or smartphones and focus on chewing food slowly and savouring each bite. This practice not only aids digestion but also enhances stomach acid production. Creating a relaxed meal environment is essential. Stress during meals can hinder digestion and reduce stomach acid production. Aim for a peaceful atmosphere to optimise digestion. You could choose to optimise meal timing and size by eating smaller, more frequent meals throughout the day. Consider having the main meal earlier (eg at breakfast or lunch) when stomach acid production tends to be higher and avoid eating close to bedtime to allow proper digestion.
Limiting alcohol consumption is beneficial as it can irritate the stomach lining and reduce acid production. Similarly, ensuring adequate sleep supports overall health and digestive function.
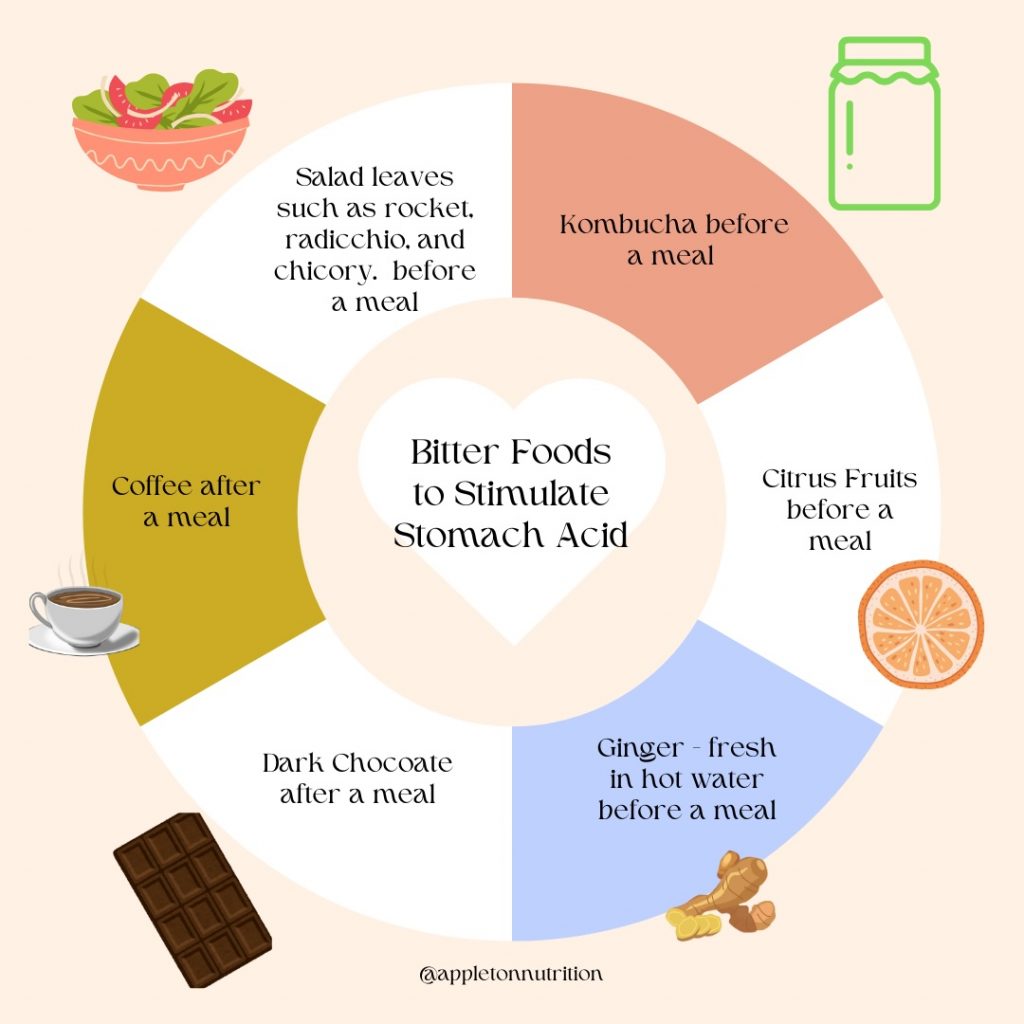
Finally, incorporate bitter foods or supplements like rocket, watercress, or Swedish bitters before or after meals to stimulate stomach acid production naturally. Kombucha that is bitter rather than sweet can also aid digestion when consumed before a meal.
By adopting these practices into your routine, you can support healthy stomach acid production, improve overall digestive function, and enhance your overall well-being.
If you know your digestive system hasn’t been right for a while, what is holding you back from making some changes? A great start is to book in for a free mini consultation with me where you’ll have the chance to talk about your symptoms and how they impact your life.
Together we can make a plan of action that might involve working with me at a deeper level and perhaps getting some diagnostic tests done.
I offer a range of packages and testing options, and I’d love to help you make the food and lifestyle changes to turn your health around.
Visit me, Nichole Appleton, via my website www.appletonnutrition.co.uk
Beasley, D.E. et al. (2015) ‘The evolution of stomach acidity and its relevance to the human microbiome’, PLOS ONE, 10(7). doi:10.1371/journal.pone.0134116.
Rinehart, A. (2023) The domino effect of stomach acid on digestion and the gut microbiome, Dr. Alex Rinehart. Available at: https://dralexrinehart.com/articles/the-domino-effect-of-stomach-acid-on-digestion-and-the-gut-microbiome/ (Accessed: 17 June 2024).
